BadgerCare Plus
Why Claims and Billing Matter
Accurate claims, and billing processes are essential for both providers and Chorus Community Health Plans (CCHP). For providers, timely and correct billing ensures they receive appropriate reimbursement for services rendered, supporting financial stability and operational efficiency. For CCHP, effective claims management helps control costs, prevent fraud, and maintain compliance with regulatory standards. Together, these processes keep care accessible, reduce delays, and build trust between patients, providers, and payers.
Claims Submissions
Claims should be processed electronically or sent by mail. Faxed claims are not accepted.
All claims must have the providers’ NPI numbers and taxonomy codes on their claims. The taxonomy on your claim must match what you have registered with the state, or your claim will be rejected. Refer to the NPI and Taxonomy Billing Requirement and Quick Reference Guide for detailed information and processes.
Allow 45 days from the date of the submission before checking the status of claims through Provider Customer Service.
For instructions on submitting corrected claims please refer to the Corrected Claims Submittal Guide.
Should you request a claim recoup or refund, refer to the Claims Recoup/Refund Request Form.
Claims Processing
New Payer ID is Required NOW
Effective February 1, 2026, any claims submitted under Payer ID 39113 will be denied.
Please ensure you are using the NEW payer ID 29123 to avoid denials and any disruptions to claims processing.
Electronic Claims
Payer Name: Chorus Community Health Plans (WI Medicaid)
Payer ID: 29123
Paper Claims
Chorus Community Health Plans
PO Box 359
Menasha, WI 54952-0359
CCHP Provider Portal
The New CCHP Provider Portal has the following features:
- Claims & claims status
- Provider appeals /disputes
- Member eligibility & benefits
- Personalized dashboard
- Explanation of payment (remits)
- In-portal messaging with provider customer service
- CCHP provider resource website links
- FAQ and more!
CCHP Provider Portal Registration Instructions guide.
Want to see the CCHP Provider Portal in action, watch the tutorial video for an overview.
Each user will need to set up their own account.
For portal assistance, call Provider Customer Service at 877-458-1289.
Availability Limited
Limited Access to Claims Look-up
BadgerCare Plus Claims Look-up Tool
- View eligibility & claim status until January 30, 2026.
- View claim payments & submitted appeals until March 1, 2026.
Provider Appeal Process
The provider appeal process gives healthcare providers the opportunity to challenge claim denials or payment decisions. This ensures fairness, transparency, and compliance with health plan policies. By submitting an appeal, providers can present additional documentation or clarify information to support their claim.
Provider should submit appeals through the CCHP Provider Portal using the Provider Portal Appeal/Dispute Process guide for detailed instructions.

Member Grievance and Appeals
CCHP members have a right to file a grievance, request and appeal and/or fair hearing. Member appeals can be requested by a member or an authorized representative, legal decision maker or a provider.
The Authorization for Disclosure of Health Information form must be completed when someone other than the member is requesting an appeal. This form is an authorization to grant those named (in form) permission to speak to the CCHP Grievance and Appeal Committee on the member's behalf.
Comprehensive member grievance and appeal information can be found in the BadgerCare Plus Member Handbook.
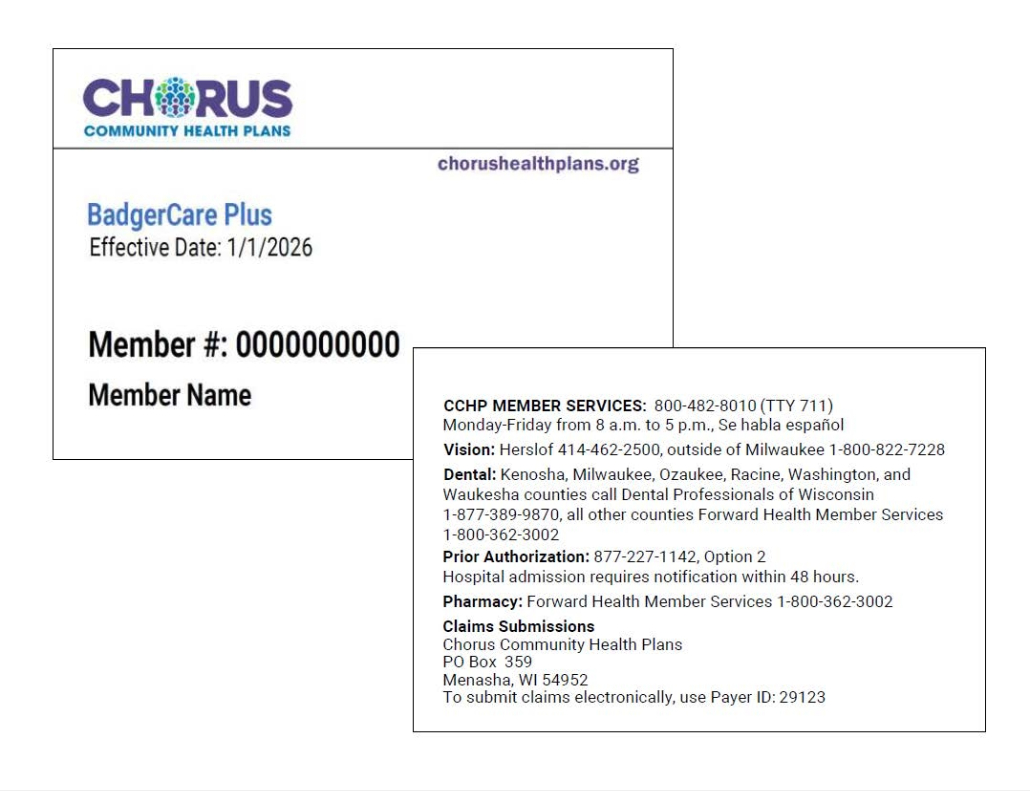
Member ID Cards
NEW in 2026, CCHP will provide ID cards to all CCHP BadgerCare Plus members. CCHP Member ID cards will be issued in addition to the ForwardHealth cards.
- Cards will be sent in wave shipments to members beginning in January 2026.
- New members and infants will have a 90-day grace period before receiving their cards.
- Care4Kids program members will not receive CCHP member ID cards.
Contact Us
For questions regarding claims and payments, contact Provider Customer Service at 877-458-1289.
For questions on authorizations, contact the Clinical Services Department at 414-266-5707 or 877-227-1142, option 2.
New TPA Administrator
There is now a new payer ID, provider customer service phone number, mailing address and EFT payment vendor with the transition to a new Third-Party Administrator (TPA) for our Medicaid line of business, starting January 1, 2026.
IFP Exit
As of December 31, 2025, CCHP has discontinued our Individual and Family Plan (IFP) product and will no longer have a presence in the Affordable Care Act (ACA) Marketplace in Wisconsin. We've set up a page of resources for providers to reference key information.
National Correct Coding Initiative
CCHP follows the National Correct Coding Initiative (NCCI) which was created by the Centers for Medicare and Medicaid. This initiative was created to stop improper coding which leads to incorrect payments.
Forward Health has implemented the NCCI to monitor all professional claims and outpatient hospital claims submitted with Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) for compliance with:
- MUE (Medically Unlikely Edits), or units-of-service detail edits.
- Procedure-to-Procedure detail edits.
MUE is the maximum units of service that a provider would claim for a single member on a single date of service for each code. Procedure-to-Procedure detail edits define pairs of codes that should not be claimed together on the same date of service.
If the claim is denied for either of these reasons, providers will receive an explanation of benefits on the remittance advice that it was denied because of NCCI.
